In the last few blog posts we have been looking at some of the pros and cons of taking insurance and then what it takes to begin taking insurance in your private practice as a counselor or therapist. In particular, we began by outlining the steps you need to take in order to get credentialed with insurance companies. Secondly, we took at look at and outlined the steps you can take to begin getting things set up to take insurance and file insurance claims for your clients.
In the last few blog posts we have been looking at some of the pros and cons of taking insurance and then what it takes to begin taking insurance in your private practice as a counselor or therapist. In particular, we began by outlining the steps you need to take in order to get credentialed with insurance companies. Secondly, we took at look at and outlined the steps you can take to begin getting things set up to take insurance and file insurance claims for your clients.
In Part 1 of this series, we talked about the three different ways to go about filing an insurance claim: using the insurance company portal, using a clearinghouse or using an EHR (electronic health record system or practice management application). Regardless of which method you use, you will still need the same information that we discussed in Part 1 on checking benefits.
In this blog post, we will look at how to actually fill out an insurance claim form and then file it with the insurance company. In the next post we will look at what needs to happen if a claim gets rejected or need to be resubmitted.
The Claim “Form”
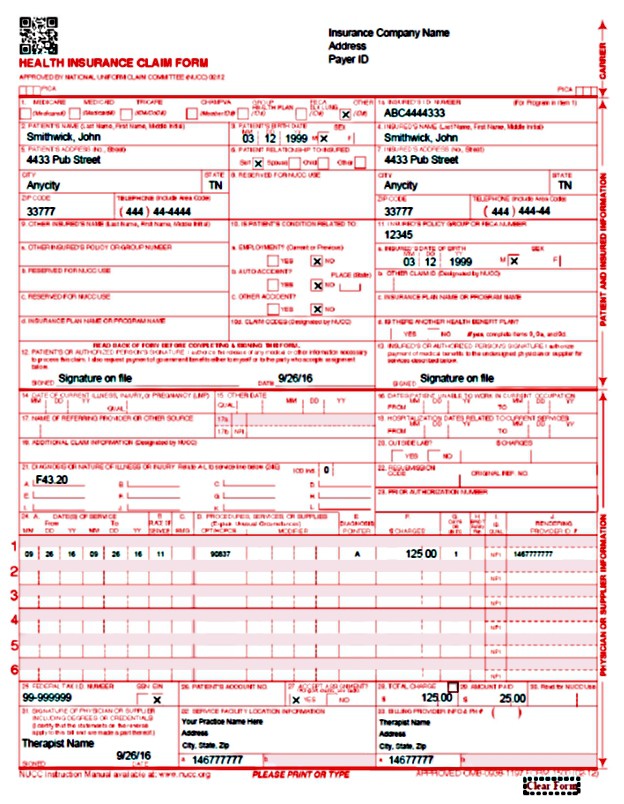
One thing to mention is that when we talk about filling out an insurance claim form, we are referring to the CMS (Center for Medicare and Medicaid Services) 1500. The CMS 1500 is the standard claim form used by practically every health insurance company in the country. And we are also referring to filling out the claim electronically rather than filling out an actual paper form. Nonetheless, it is helpful to use the paper form as a guide.
The CMS 1500 is broken into 33 sections of information. The good news is that you do not have to fill out every section on the form in order to file a standard health insurance claim. Most of the time, the when you are completing a form online at your computer, only the required information is asked for. This is especially true if you are using the insurance company portals or a practice management systems specifically made for mental health practices.
In the top right corner of the CMS 1500 is where you enter the information about the insurance company. Obviously, if you are using the insurance company portal, this information is not needed. But if you are using a Clearinghouse or EHR, you will need to enter this information. Most of the time, you will only need the insurance company name and their Payor ID. This is the universal code, kind of like an NPI number, that is used by clearinghouses and EHR systems to identify the insurance company.
What goes in each section
In sections 1-3 and 5 are pretty self-explanatory which is your client’s (patient) information. Be sure to double and triple check the “Insured’s ID Number” in section 1a. If it is wrong at all, the claim will be rejected. (That’s why it is important to get a copy of the client’s insurance card).
Sections 4, 6, and 7 are information about the “insured”. This is very likely to be the same as the client’s information, but not always. An example would be the spouse or parent of the client is the insured and the client is on their health insurance policy.
Section 10 – answers are usually answered “No” for most mental health claims.
Section 11– is where you enter any Group Number if there is one. If not, either leave blank or enter in “none”.
Section 11a – is self-explanatory; insured’s date of birth and gender
Section 12 & 13– you would simply put in “Signature on file” and the date of the first visit.
Section 21– enter the primary DSM diagnosis using the ICD-10 code on line A. If there is more than one diagnosis, you can fill them in on lines B-L. (You only need one diagnosis though). In the top right of this section there is a space labeled “ICD Ind.”; just use 0 to let them know you are using ICD-10 (Most all the insurance companies are now using this anyway).
Section 23 sometimes if services require a prior authorization, like with an EAP claim, you would enter the authorization number here. If no pre-authorization is needed, just leave this section blank.
Section 24a enter the date of service; same date in both “From” and “To”. Be sure to put the date in both.
Section 24b place of service which is nearly always “11” which simply means your office.
Section 24d is the CPT Code for the session. CPT means, “Current Procedural Terminology” or simply the type of session you had. For mental health the most typical codes uses are:
- 90791 – Initial diagnostic and interview
- 90837 -60 minute individual psychotherapy session
- 90834 – 45 minute individual psychotherapy session
- 90832 – 30 minute individual psychotherapy session
- 90847 – Family therapy with patient present (90846 w/o patient present)
- 90853 – Group therapy session
Section 24d also has a section for “Modifiers”. Most of the time these are not used. But when required, they usually are two letters and might be specific to the insurance company. Some common ones are:
- HO- Master’s level therapist
- AH – Clinical Psychologist
- AJ- Clinical Social Worker
- HP -Doctoral level therapist
- GT- Teletherapy or online session
Section 24E is usually “A” which is the diagnosis code line from Section 21 that you are working on for the session, you could add several letters if needed or appropriate; eg. A,B,C etc.
Section 24F enter your charges for the session. Tip: Put your full rate here not just the contracted rate with the insurance company. That way the insurance company and the client know the “discount” you are getting. Also, plans can vary within insurance companies and you might get more for a particular type of session or plan.
Section 24G this is nearly always 1 unit
Section 24J your NPI number
Section 25 your tax ID number
Section 27 check “Yes” to have payment of the claim to come to you.
Section 28 total charge from section 24F
Section 29 any co-pays or payments the client made
Section 31 your name and date
Section 32 & 32a; your office location and address; the NPI number will depend on how you are contracted with the insurance company. If you are in a group practice be sure and put the group name and address here. If you are a solo practitioner, you would simply put your name and address here.
Section 33 & 33a enter the name of your practice. Again, the NPI number will depend on how you are contracted with the insurance company. If you are in a group practice and the payments need to come to the group, be sure and put the group name and address here. If you are a solo practitioner, you would simply put your name and address here.
The good news is that the rest of the sections of the claim form are rarely ever used for mental health claims. Once you have the above information entered, the claim is ready to file. Do go back and check to make sure you have entered your information correctly. It is very easy to leave out a digit in one or more of the numbers asked for. This one reason why I recommend using a clearinghouse because with the “scrubbing” they do automatically alerts you to any missing or wrong information before it is submitted to the insurance company. Again the Clearinghouse that I can recommend is Office Ally. It’s free to sign up for use unless they send out a paper claim for you which they do charge for.
In our next post, we’ll look at how to handle rejected claims and how you can quickly correct claims and resubmit them.
Other great resources:
The Insurance Answers Podcast
The Insurance Billing and Credentialing For Mental Health Clinicians Group on Facebook
 By L. Gordon Brewer, Jr., MEd. LMFT – Gordon is the President and Founder of Kingsport Counseling Associates, PLLC. He is also a consultant and business mentor at The Practice of Therapy. Follow us on Twitter @therapistlearn. Join the Facebook Group.
By L. Gordon Brewer, Jr., MEd. LMFT – Gordon is the President and Founder of Kingsport Counseling Associates, PLLC. He is also a consultant and business mentor at The Practice of Therapy. Follow us on Twitter @therapistlearn. Join the Facebook Group.