Nearly 1 in 5 adults experience a severe mental illness in their lifetime. Dr. Tom Young is a physician, and he has developed a screening tool for other professionals in the health industry. The tool helps physicians realize when they need to refer out to mental health providers. I’m looking forward to you hearing from Dr. Tom and learning about the technology that he’s put together with his team at nView Health. Plus, we chat about the use of innovative technology and data insights to positively impact all those who serve this vulnerable population.
Meet Dr. Tom Young
 Dr. Tom Young is the co-founder and chief medical officer of nView Health, an innovative software company that helps you better identify, treat and monitor patients with behavioral health conditions, featuring the world’s most trusted digital assessment – the M.I.N.I.
Dr. Tom Young is the co-founder and chief medical officer of nView Health, an innovative software company that helps you better identify, treat and monitor patients with behavioral health conditions, featuring the world’s most trusted digital assessment – the M.I.N.I.
Primary care physicians make 80% of diagnoses and decisions around behavioral health and get it wrong 92% of the time. nView’s suite of online behavioral health solutions empowers primary care physicians, pediatricians, behavioral health practices, psychiatrists, therapists, and counselors who specialize in identifying and treating patients with mental health, substance abuse, and other behavioral health disorders to get it right 98% of the time.
Intersecting Mental & Physical Health
Most family physicians find that there is so much more to their patients than physical health. Of course, there is always the mental aspect of our health. Like most young physicians, Dr. Young was not taught much about mental health back in those days. However, Dr. Young taught medicine for several years, and in those adventures, he began to think more about it. All along the way, he started to understand the depth of opportunity that needed to happen between primary care providers and people’s mental health providers. So, Dr. Young began his journey on finding ways to intersect those two worlds, hence nView Health.
The Mental Health Covid Crisis
The concept of mental health has really changed over the last 12 months because of the pandemic. The mental health tsunami behind the pandemic increased anxiety and increased depression. Now, mental health professionals are trying to keep up with the demand. Sadly, it’s affecting all ages of people, and we’re seeing children needing mental health assistance now a lot more than before. Unfortunately, more than 5 million children in America have some serious mental illness that significantly interferes with their daily lives.
The critical issue for primary care is getting the proper initial assessment. However, if a doctor doesn’t know what to look for, they will not be able to spot an issue. So, Dr. Young provides a tool that’s quick and easy. It only takes a couple of minutes for the patient to fill out, and it really lets the primary care provider decide where they should focus their energy. Dr. Young’s Mini International Neuropsychiatric Interview (M.I.N.I.) — has been used in patient care and clinical research for more than 25 years.
Coordinating Mental & Physical Care
For the most part, primary care providers want to understand how their patient is doing. Like any other referral process in medicine, doctors will send their patients to you with the hopes that you’re able to help them. Then, the patient will come back in between for something medical. That doctor should be able to converse with them about their progress with you in that visit. However, if the doctors don’t know what’s going on, they will feel left out of the healing process. Then, that’s where some of the fractured relationships occur. Sadly, doctors will send a patient for care and then never hear back. Some ways to coordinate care are through phones, tracking tools, and assessments.
Using Data As A Therapist
Dr. Young’s daughter is a therapist; she found that this assessment tool was great for her work. First, she gets to provide data back to her referring physicians. Plus, she can see how her practice is doing. As she grew her practice using the interview tools, it gave her greater confidence in each therapist’s diagnostic skills. It’s a beautiful tool because therapists want to know if their patients are getting better. Well, how do you know that? If you use a tracking tool attached to the right assessment tools, you have the data that shows you what’s going on. While on the other hand, you’ll have the data to know if your patient is, in fact, not getting better and maybe needing more assistance.
Gordon Brewer 0:00 this is the practice of therapy podcast with gordon brewer helping you to navigate your private practice journey this is session number 171 of the practice of therapy podcast hello everyone i'm gordon brewer glad you've joined me hope you're having a good week or weekend whenever you might be listening to this and i'm so glad you're with me on this journey um you know i'm pretty excited today you know as usual i record most of the intros and outros for my podcast on fridays and today is one day i wish i wasn't inside it is absolutely gorgeous here in east tennessee and spring is here and things are budding you know that it's a sign of spring when as we call them here in east tennessee the red buds are blooming in it so you know i think there are a lot of different names for the trade but that that is what we know it here in east tennessee but anyway it's it's a beautiful beautiful day so i just thought i'd share that i'm looking for you looking forward to you rather you hearing from my guest today dr tom young and dr young was a person that had reached out to me a few few months back but he is he is a physician and he has developed a screening tool for other physicians and just helping them with looking at what when they need to refer out to mental health providers and so i thought this is a great topic and certainly perfect for the ira niche here as you listen to this and so i'm looking forward to you hearing from him and the the the tools that he's put together with his team he's the founder of inview health and so you're going to get to hear from him and learn more about his story and the tools that are that they're providing you know one of the things that i will say before we get to get to the interview is that one of the i remember back when i first went into private practice one of the best ways to get referrals i think was from physicians in my area and just being able to reach out to them and let them know that i was taking new clients and and all of that and so anyway i'm looking forward to you hear hearing from dr tom young here in just a moment but before we get to dr young i'd like for you to be sure and go over and check out the google workspace for therapists course so here is the deal i'm getting ready to close the cart on that while i finished the updates on the course so you have until the end of march march 31 2021 to go ahead and get that course at its original price i'm going to close the cart so i can finish my working on the updates for it but when you purchase it you will get the updates and you'll get even though it closed the cart you'll still have access to the course it's just that new people won't be able to buy it for a while until i get those updates so wanted to make you aware of that and the price is going to go up but currently you can still get the course for $98 and what the course does is essentially teaches you how to use the different tools and some hacks and that sort of thing for using google workspace within the private practice context and in particular learning how to make it hipaa compliant and hipaa secure and then being able to use it as a practice platform in particularly the business side of your practice so anyway be sure to check that out and you can get to that by just going to practice a therapy.com slash g suite course that's still under the old url before google changed the name to google workspace but it was formerly known as g suite so anyway be sure and check that out and take advantage of getting it at its original price before the price goes up here in a few months So, just wanted to give you a heads up on that, if you're on my email list, you would have gotten a notification about that. But we're running out of time here, folks, it's just a few more days till the end of our March, which is hard to believe, in and of itself. So be sure and check that out. And before we get to my conversation with Dr. Tom young, I'd like to invite you to go over and check out our sponsor for the podcast, therapy, notes, therapy, notes, calm. They are the leading Electronic Health Record system for mental health providers in private practice. As I've mentioned before, they are who I use in my practice, and it is just a wonderful tool for me, and I can't say enough about them. It is it is it really contains everything you need, in terms of documentation for your practice, also scheduling, being able to use telehealth within the same platform, also, being able to Bill insurance companies, and do electronic claims through all through therapy notes. Also, their support is just second to none. They are responsive and will absolutely help you with any problems you might run into. We recently added a therapist and we had to transfer their records from a previous pack practice. And they did it all for us at no extra costs. So it's a wonderful tool. And I highly recommend them. So be sure and check them out therapy notes doc.com. And if you'll be sure and use the promo code Gordon, just g o r d o n, you can try them out for two months for free. So it's really a win win situation. So be sure and check them out. Therapy notes calm. And so without further ado, here's my conversation with Dr. Tom young. Well, hello, everyone, and welcome again to the podcast. And I'm so excited for you all to get to know Dr. Tom young. And Dr. Duck young Dr. Tom reached out to me about being on the podcast. And when I started learning about what he's involved in from, particularly from the medical perspective of helping doctors connect with behavioral health providers. And just some of the things that have come up over this past year. I knew he was a guest that we'd want to have. So Tom, welcome to the podcast. Dr. Tom Young 7:49 Gordon Brewer 7:53 Dr. Tom Young 8:06 at and what I found is most family physicians find is that, you know, there's there's always the other part of people besides their physical or medical health, and that's their, that's their mental health, behavioral health, their emotions. And like most young physicians maybe was not as well schooled back in those days. I taught medicine for several years, and in those adventures began to think more about it. And all along the way. For all the things I've done have been sort of beginning to really understand the depth of that I had the opportunity to be the medical director for Medicaid for many years for the state of Idaho. And in that position, I really began to see the interaction between primary care providers and people's mental health. And so I started my journey into looking about how to make that better, how to make that something that physicians could do. And that's what brought me to found in view health is a way to create tools for primary care physician pediatricians, nurse practitioners, pa there, we're seeing people in the trenches. It came from the concept that primary care providers provide about 85% of all the diagnoses and mental health in this country today. They write about 80% of all the prescriptions for psychotropic drugs. And unfortunately, their rate of getting the actual diagnosis is relatively low. Not because of any intent, but because we really haven't provided tools to help right right Gordon Brewer 10:04 Dr. Tom Young 11:23 Gordon Brewer 14:50 Dr. Tom Young 16:08 Gordon Brewer 18:14 Dr. Tom Young 19:04 Gordon Brewer 20:26 Dr. Tom Young 20:58 Gordon Brewer 21:50 Dr. Tom Young 22:55 Gordon Brewer 26:07 Dr. Tom Young 27:02 Gordon Brewer 27:57 Dr. Tom Young 28:34 Gordon Brewer 30:29 Dr. Tom Young 30:40 Gordon Brewer 32:20 Dr. Tom Young 32:54 Gordon Brewer 33:56 Dr. Tom Young 34:11 Gordon Brewer 35:02 Dr. Tom Young 35:23 Gordon Brewer 35:57 Dr. Tom Young 36:07 Gordon Brewer 36:20 you have been listening to the practice of therapy podcast with gordon brewer please visit us at practice of therapy.com for more information resources and tools to help you in starting building and growing your private practice and if you haven't done so already please sign up to receive the free private practice startup guide and practice of therapy.com the information in this podcast is intended to be accurate and authoritative concerning the subject matter covered it is given with the understanding that neither the host guests or producers are rendering legal accounting or clinical advice if you need a professional you should find the right person for them
this episode of the practice of therapy podcast is brought to you by therapy notes therapy notes.com and also the google workspace for therapists course again you can find that at practice of therapy.com slash g suite course
Oh, it's a pleasure to be here, Gordon. I really looking forward to the conversation.
Yes, Yes, me too. So. So as I begin with everyone kind of tell folks, kind of how you've landed where you've landed and your journey and a little bit more about yourself.
Great, happy to do that. Now my journey started in medicine, particularly in family medicine, where I came to where I live now, which is Boise, Idaho, from Texas, where I trained
yeah yeah i love this concept because i think a lot of times i know even my own practice will get referred first of all i think that one of the things that is particularly for those of us in the mental health space particularly for those of us in private practice one of the things that i've really kind of discovered once i got into private practice was is that a lot of doctors out there really are sometimes struggle in finding who to refer to and and they see that with their patients they have some mental health problems or some behavioral health problems and just knowing how to steer their patients in the right direction and then just that cold communication between the therapist and and the doctor is such an important piece but what are how are you finding that a lot of doctors are kind of broaching this whole thing because i know one thing that has happened over this past year is that mental health has become an ok topic for people to talk about as a result of COVID and all of this sort of thing
yeah you're absolutely right gordon the concept of mental health has really changed over the last 12 months it's become a part of the pandemic part of the essence of the pandemic it's what i call sort of the tsunami behind the pandemic increased anxiety increased depression increased notice a behavioral health is work at all age brackets characteristically we really don't think too much of children aged you know when the young ages but we're seeing with children now a lot more than before and in our work and in view we work with a lot of groups who are now focused on things like anxiety for children and working to find solutions but i think the the really the key issue for primary care is getting the right initial assessment it's kind of what we call the tip of the spear because if you don't know what you're looking for and you don't know what it is and you don't don't have a way of initially finding it how do i screen people in my practice there are some screeners out there unfortunately most of them are focused on the symptoms so it really doesn't help the primary care doctor essentially understand what are my options give me an example if i think the patient's depressed that may be my level but i really don't think about the fact that this might be depression with psychosis this might be depression it's bipolar it could be a depression secondary to ptsd i really don't get that depth in the current assessment tools so what we focused on is providing a tool that's quick and easy takes a couple of minutes for the patient to fill out and it really lets the primary care provider whether it's pediatrician because we have children's versions find out what might be going on and with that finding out what might be going on now i know what to focus my energy on now i now i find out who might be the best provider in my community for that so in terms of how we interact them with the behaviorist in our community we have to be able to tell them what we think is wrong have them start their their intervention process and then together we need tools that follow along how is my patient doing how is what's the progress so we focus on that spectrum of assessment initial sort of diagnostic tools to help physicians make the diagnosis the tools themselves don't make the diagnosis but they provide information i like people to think about what we do is kind of like the standard of what we as primary care doc's do you come in you tell me what's wrong i focused on a particular possibility of what might be going on and i order some appropriate tests maybe it's an ekg maybe it's an x ray and i get that back and that helps me focus what i need to do next same things true here
yes yes i love that concept because i think a lot of times what what can happen is as i know we can First of all, I'm a big proponent of coordination of care with, with the medical with the medical side of things. And, you know, I know, having worked in an agency in the past, one of the things that is so important in getting when we get patients as is that we get them medically cleared, you know, just to rule out any sort of, you know, some sort of underlying medical condition that could be causing things, you know, one that comes to mind is just if somebody's got a, say, for example, a thyroid condition that can present is something, but you know, just depression and flat effect, and all of that kind of stuff, and, you know, really needs to be ruled out in. And just on our side of things, what, what have you found that, in that cold coordination of care, and I want to, I want to get to here in a minute, a little more detail about how this assessment works. But from, what do you find that most doctors are looking for in being able to coordinate care with mental health providers,
I think for the most part, primary care providers want to understand how their patient is doing. Because it's like any other referral process in medicine, I send my patient to you with the hopes that you're able to help them, they come back in in between for something medical, I want to be able to converse with them about their progress with you in that visit, but if I don't know what's going on, I feel left out. Right. And I think that's where some of the fractured relationships occur. You know, I send that patient to you, and then I never hear back. And I think to coordinate care, there are a lot of ways to do that. It can be by phone call, we can discuss the pain, you may use tracking tools, things to assess the patient in between visits, sending me a copy of those, so that I can see that my patient is getting better. Yeah, are very valuable. And so I think all of those things are what we talked about when we say coordinate care. The other part that I think's important is if I'm using medications, then I need to understand if you're seeing any of the side effects, perfect example, I decide based upon what I found out about the patient and my diagnosis that they are depressed, there may be an 18 year old or 19 year old college student, and I give them a medication. That was many people know, some of these medications will drive suicidal thinking. So I need to coordinate with you, who's seeing this patient maybe every week, to understand is that going on? Are those questions being asked? So that you and I together can be careful with the patient. So I think that's where it comes in.
Right. Right. Yeah, I think that's a, that's a such an important piece. Because I know, one of the things that I know, again, in just thinking about my own practice, I know when when we first do an intake with a with a patient, it might be that it's going to be helpful to know if they are on any medications and and also being able to refer back to to their doctor. You know, if we feel like they could be maybe benefit from some medication. D, do you find that that's happening a lot with patients were just what your work with other doctors around the country, that their therapists are referring them back to the doctor for those things.
I think that happens a lot. I think that and that's a very appropriate relationship between physician and therapists. And I know more and more primary care providers are beginning to even integrate therapist into their practices. You know, particularly in areas like Federally Qualified rural health clinics, if qH sees a lot of Fq HCS, around the country and rural areas will integrate the therapist as part of the office, if you will. So I think those those relationships are beginning to build. I think we're seeing, as you mentioned earlier, a greater emphasis on integration of behavioral health and physical health, right? Both both physically where people are moving into the same space and in the referral process. And again, when I, as a primary care provider can get more information that says this, there is an issue here, you know, I do that screening and there is a documentable issue, then I can be more aggressive, if you will, about helping that patient find the right therapy and find the right person to match with their problem, if
you will. Right. Right. Yeah. What did you know, one of the things too, I would imagine, on the medical side of things is, is doctors feeling more confident about, you know, what they're diagnosing, but also being able to prescribe appropriate medications for different different conditions? And are you finding that with, in view, in view application that they're feeling more confident about that?
Well, I think so i think if i can understand that my patient has, and I'll say a simple uncomplicated depression. And, and does not have, for example, bipolar disease, there are no other comorbid conditions. Often we see depression, as you will know, in your practice, that really comes from other things, it may come from significant PTSD. There may be, particularly in adolescence, that depression may man may come from an underlying eating disorder, for example. So by primary care providers being able to understand the complexity of this individual patient, they can feel more confident in the medications that they may choose.
Yes, well, the one thing that seems pretty evident to me is that, you know, we had talked earlier about the fact that some of the stigma around mental health, it seems to be you know, I haven't really, I don't have any way of measuring abeja seems to be kind of dropping, because most everybody around the COVID pandemic has felt a significant amount of stress around that, having to socially isolate and all of that social distance and isolate and all that sort of thing. And I think that people are probably more quick to, to go to their primary care doctor to talk about these things. And they might be to seek out a therapist. And so to me, it's a perfect solution to helping people get the help that they need around that. So you want to talk a little bit more about in view and how it came about and kind of what's up how, how doctors are using it?
Well, how it came about is I was my wife and I were working in Florida, and we met Dr. David Shanahan, who was succot well known psychiatrists to over the years have developed assessments that were used in the research world. And they still are our company provides significant amount of assessment tools into the worldwide research. Today, we have research projects going on every continent 1000s of tests a day are done. And I as a primary care doc, and as somebody sort of in that space, looking at healthcare in general, I saw the opportunity to move some of these tools by Dr. Shanahan by Dr. Wayne Goodman, Dr. Katherine Phillips, several well known psychiatrists and move them into a format or delivery model that could allow primary care doctors to use them. Because they were devoid of tools. There were a few screeners, but the ability to provide a sharp psychiatric interview at the level of the primary care doc which would give them the information and I laughingly when I started this as well, this is kind of like having a psychiatrist in your pocket. And I wanted to give primary care Doc's that availability. So we started with a screener, which which often opens the conversation between the doctor and the patient. I give the patient a screener, it comes right back, I can look at it and say, Wow, Mr. Jones, looks like you may be feeling you know, a lot of anxiety, is that something that we need to talk about? So it changes the paradigm of the patient having to complain up and puts the puts the onus in the physicians hand to know what's going on and ask the right question, and then once they do that, the next step in the toolbox Assess is the interview that I can quickly do with the patient. That helps me if you will drill down and get a more accurate picture. Once I have that accurate picture, I can then find out with you as a therapist, or if it's going to be medication, what our next steps. And then lastly, the tools are generated to be able to provide those tracking tools to say, how is the patient doing if I choose medication, if I choose medication, and therapy, and I can see how that patient does weekly, monthly, however often I want to track it. And then as the primary care provider, I have more knowledge to be able to work with the therapist, if we're not seeing improvement, is it a medication change? Is it adding to the therapy? You know, do I need to move to from pure cognitive behavioral therapy, perhaps to cognitive behavioral therapy with some TMS, trans magnetic stimulation, so I can look at things better and see better outcomes? Right. Right.
Well, it's, yeah, it's the fact that it's just database, I think it really is, gives it much more, really much more to work with, I think, on the front end, by just having those, you know, those assessments that are based on science, if you will, I think is just huge in terms of, of helping come up with an accurate diagnosis. And, you know, the other thing that occurs to me is that I think a lot of times, and I see this for people coming to therapy is that they, they feel something is amiss, but they can't quite pinpoint what it is. And by having an assessment, I think it really helps them have the language to really express what is going on for them internally. So
I absolutely agree with you, 100%. And you know, what we could what's the catch, we're now measurement based care. But measuring and tracking is also therapeutic. It's the patient begins to get engaged and see that things are getting better often. It's kind of like if if you live in the darkness, you can't see it as subtle changes in the light. Right. And so sometimes tracking together with their therapy becomes therapeutic. And so I think there's, there's not only is it measurement based care from the outside you and I looking at at our performance, doctor and therapist, but it's also the patient looking at how they're doing and being able to say, Yeah, I really am getting better.
Right, right. Well, that's, it's, I love this idea. And I'm really excited about the the potential for this not only not only for helping helping our patients, our clients, which is, you know, for most of us, that's our primary concern, but also for being able to, to build a practice more by having more communication with with doctors along the way. Do you see that this this particular application would be helpful for therapists are people doing more the talk therapy into things?
Absolutely. Our use a family story, if I can't, my daughter is a therapist. And as we got into this, she found that this was a really great way. Number one for her to provide data back to her referring physicians, but also for her to see how her practice was doing. And as she grew her practice, using the interview tools, having her therapist use the interview tools, it gave them greater confidence in the accuracy of each therapist diagnostic skills, wow. And and in the college practice that I have same thing is true. By using the interview tools in the screening tools, we're able to much more rapidly and at a higher level of quality. start the process with each individual patient. So for therapists, I think it's a wonderful tool, because again, therapists, like physicians in the new world are going to be measured on outcomes, or the patients that you see getting better. Right? How do you know that? Well, if you use a tracking tool that's attached to the right assessment tools, you have the you have the data that shows you what's going on. And conversely you have the data that shows you If the patient isn't doing better, which then you as the therapist or me as a physician can make adjustments. Right quickly in what's going on. So yeah, I think it's it we have numerable number of therapists to use the tools in their practice. Yeah. And, and a growing number, but again, because it's efficient, gets at the information, collects the data quickly, collects it accurately, and then allows the therapists to follow over time, right.
And I would imagine that you get the kind of a provisional kind of diagnosis it just immediately with the with the tool,
yeah, it takes about if you do the screener takes about two to three minutes, we also throw him, we also all of our tools are the only ones in the world currently, that go all the way down to age six, while we're assessing children from six up. And so if you do the screener, it's about two to three minutes, you can do the full mini in the adult, which has 17 DSM five modules, that takes anywhere from 20 to 25 minutes, and in 90 seconds, you have a report back that tells the provider all the conditions that the patient meets the DSM criteria for Wow. And you have all the independent answers, so that you can dig into areas that the patient may may have said yes to and again to sort of quickly initiate the discussion around the problem areas. And then the tracking tools each probably take less than a minute and a half. And they can be sent out to the patient via email. And they can answer them on their phone or their watch, or any number ways to let you know how they're doing in between. So they're quick, they're efficient. They're extremely accurate. They've been validated, over 25 years, and are still constantly used today as one of the leading assessment tools in the world. So we feel comfortable that when people use our tools, they're getting good information. They're getting information that they can depend upon, and it can help them help their patient. That's really the key for us.
Yeah, yeah. Well, I think it's a, it's, it's amazing, being able to have kind of that leg up in just being able to know how to quickly work with, with clients and patients. What I what really stuck out for me about what she said, is just being able to look at how they answer the questions, and really kind of being able to hone in from there about, okay, this is something they've they've not mentioned before, but they answered this question in a particular way. How to, you know, let's dig in a little deeper into this. Yeah,
it's exactly right. And often, when when people and you can deliver the you can do these administrations couple of ways you can, you know, actually hand the patient a tablet to answer these in your, in your office, you can ask the questions in the office as part of your interview. Or you can email the tools out in advance. And that's what we do, we get to college a lot. And then when the patient shows up, we automatically already have a diagnostic interview completed. So our therapists can begin right away to hone in on those key issues. And there's no sort of searching. I know right away, this patient has anxiety, this patient has depression. And those are things that I can look at the as you say the answers to the question. So it's it's a, it's a very efficient way to get the information from people in a timely way. Right,
right. Oh, this is great. This is great. Well, I know that people will be interested in how they can find out more, Tom. And also I want to be respectful of your time. tell folks how they can get in touch with you or find out more about Nv?
Well, you can go to any view in the i e w.com. All the information is there about us and how to get ahold of us. We have a strong team of people. We have a strong clinical advisory group. We're there to help people like primary care Doc's therapists, and others really get the right information. So we have a great staff of people. Wonderful folks who are happy to answer your questions. We have a process on the website. So if you have a question, it's going to be generated that that moment right to somebody on the staff to be able to reach out to you either by phone or by email, however you wish to be contacted. and then we can provide you information
awesome awesome and we'll have links in the show summary and show notes for all of this so people can find it easily so tom welcome any other parting thoughts you have for us and just thinking about you know this whole coordination of care between the medical side and the therapy side and in all of that
i think the last thing that i really appreciate the opportunity because i see this integration between therapists and physicians particularly primary care doctors as really key because the backstop for mental health in this country has become the primary care providers and their ability to then help their patient get the therapy that they need through therapists like yourself that's really going to be life changing in this country for the concept of mental health so
i appreciate the opportunity to talk about awesome yes and i'm so glad you joined me on the podcast and hopefully maybe we'll have some more conversations in the future
i would look forward to it
well i'm very grateful to dr tom young for joining me on the podcast and one of the things that i learned you know early on when i first went into private practice is that your doctors and your primary care providers can be a wonderful resource for you particularly you know and getting referrals and that sort of thing and i think to be able to share with them tools and that sort of thing they're always looking for those i know i've got several friends that are primary care physicians and one of the things that they're always looking for is people to refer to when they when they figure out that that i that a patient of theirs has some mental health issues that can benefit from from therapy so i'm so grateful to dr young for being able to create the tools that he has and you can check it out at in view health and org again there'll be links here in the show notes in the show summary for you to find out more about that and how you can maybe see how about integrating that maybe as a to with your own practice so again i'm glad that you join me for the podcast and be sure and check out the google for google workspace for therapists course before the price goes up at the end of this month of march 3 march 2021 the as i had mentioned earlier on putting some updates in for the course and i'm going to close the cart at the end of this month march 2021 and get those updates completed but if you purchase it now you'll get it at the original price plus you'll get all the updates show get those live and you also have lifetime access to the course and in the course you're going to learn about the different tools of google of google workspace and how you can use them in your practice for making you more productive and helping you manage the whole business side of your practice so be sure to check that out at practice of therapy.com slash g suite course it's under the old url still but we'll get that updated here soon that should be sure and check it out also be sure and check out our sponsor for the podcast therapy notes therapy notes.com they're the leading electronic health record system for mental health providers in private practice they're who i use in my practice and i'm absolutely thrilled with that that they serve as they provide but also how it keeps our practice running smoothly with both with scheduling and appointment reminders also the payment payment portal there is also telehealth included in the package that you get from therapy notes and it's it's well worth the investment so be sure to check them out and you can you you can try them out for two months for free if you'll just simply use the promo code gordon just glr d o n again therapy notes.com well folks thanks again for joining me for the podcast i'm hoping you're having a good week or weekend whenever you might be listening to this i'm just thankful that springtime is finally getting here and we're almost out of march already that's hard to believe this month just flew by but the warm weather is returning at least here where i'm living and yeah and it's just exciting so anyway take care folks be sure to subscribe to the podcast if you haven't done so already and leave us a review always anxious to get honest feedback about the podcast and be sure and share with your friends so take care folks and we'll talk to you next week
Being transparent… Some of the resources below use affiliate links which simply means we receive a commission if you purchase using the links, at no extra cost to you. Thanks for using the links!
Dr. Young’s Resources
nView Health
Young Healthcare Consultants
Resources
 Use the promo code “GORDON” to get 2 months of Therapy Notes free.
Use the promo code “GORDON” to get 2 months of Therapy Notes free.
Google Workspace for Therapists | The E-Course
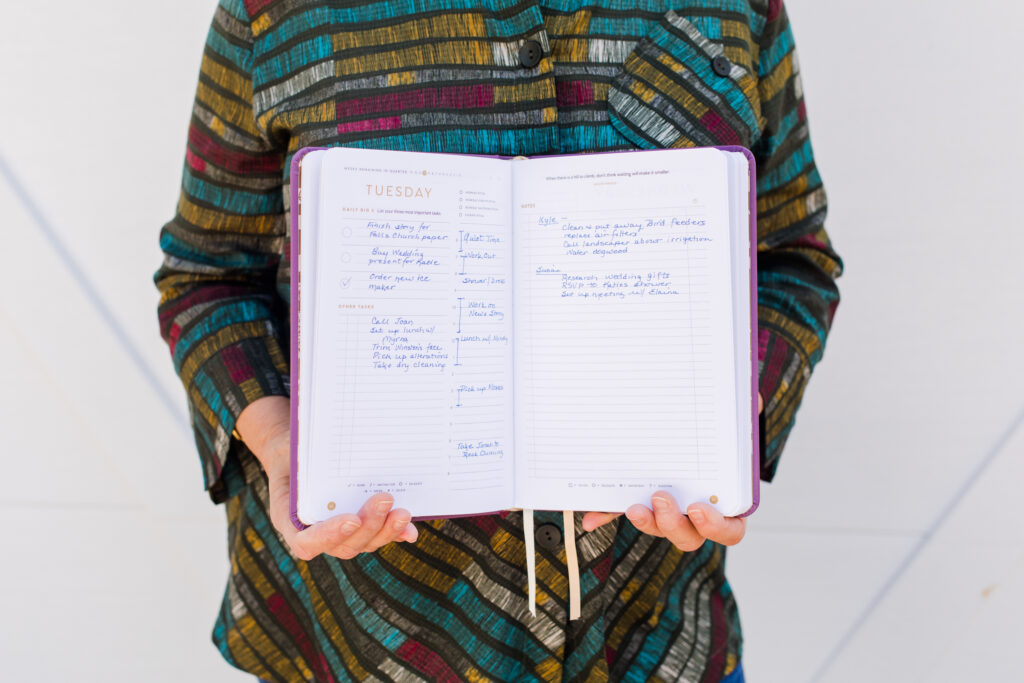
Purchase The Full Focus Planner™
Join my Focus Groups
Session Note Helper 3.0
Money Matters in Private Practice | The Course
Join the Google Workspace (formerly G-Suite) for Therapists Users Group
Cool Resources
Follow @PracticeofTherapy on Instagram
Meet Gordon Brewer, MEd, LMFT
 Gordon is the person behind The Practice of Therapy Podcast & Blog. He is also President and Founder of Kingsport Counseling Associates, PLLC. He is a therapist, consultant, business mentor, trainer, and writer. PLEASE Subscribe to The Practice of Therapy Podcast wherever you listen to it. Follow us on Twitter @therapistlearn, and Pinterest, “Like” us on Facebook.
Gordon is the person behind The Practice of Therapy Podcast & Blog. He is also President and Founder of Kingsport Counseling Associates, PLLC. He is a therapist, consultant, business mentor, trainer, and writer. PLEASE Subscribe to The Practice of Therapy Podcast wherever you listen to it. Follow us on Twitter @therapistlearn, and Pinterest, “Like” us on Facebook.